Schizoaffective Disorder Medications
Schizoaffective disorder is difficult to diagnose because it includes elements of both schizophrenia and a major mood disorder. Consequently, treating it requires a multifaceted approach as well. Because it involves the occurrence of psychotic symptoms, there’s a need for medication as part of the treatment plan. At URP Behavioral Health, the inpatient treatment program includes evidence-based and holistic therapies in combination with medication.
Each medication plays a different role in managing schizoaffective disorder symptoms. The main classes are antipsychotics, antidepressants, and mood stabilizers.

Antipsychotic Medication
Antipsychotics are the first type of schizoaffective medications that are prescribed when you receive a diagnosis. Although they don’t cure psychotic symptoms like hallucinations or delusions, they help you control them, which reduces stress. When you’re able to manage these symptoms, you become more responsive to other types of therapy.
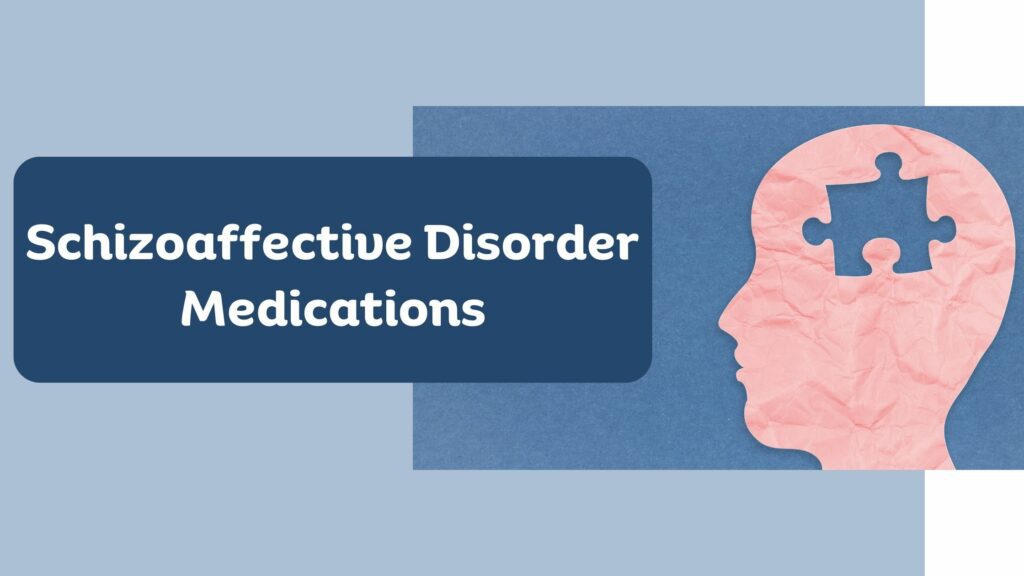
There are two types of antipsychotics, and the type you receive will depend on your symptoms.
Typical Antipsychotics
Research indicates that psychotic symptoms occur as a result of excessive D2-receptor stimulation. It suggests higher levels of phasic activity among dopaminergic neurons in the subcortex. Another study states that according to the ‘original dopamine hypothesis,’ schizophrenic symptoms are the result of hyperactive dopamine transmission. Therefore, typical antipsychotics, also known as first-generation antipsychotics, work by inhibiting dopaminergic neurotransmission.
Some of the common drugs that fall under this category include dibenzoxazepines, butyrophenones, and phenothiazines. These medications are associated with some side effects, such as insomnia, dizziness, confusion, and sedation. Some people also experience extrapyramidal symptoms like bradykinesia (slowed movement), dyskinesia (involuntary and erratic movements), dystonia (involuntary muscle spasms and contractions), and akathisia (the inability to stay still).
Atypical Antipsychotics
A common feature between typical and atypical antipsychotics is that they work by blocking dopaminergic neurotransmission, i.e., blocking the D2 receptor. Second-generation antipsychotics have the additional effect of blocking serotonin receptors. That’s because serotonin dysregulation could be a potential reason for negative symptoms that are part of the schizophrenic criteria. It also contributes to feelings of depression that commonly occur in people with psychotic disorders.
Therefore, atypical antipsychotics help alleviate both positive and negative symptoms. Keep in mind that positive symptoms refer to the changes in perception that are added to your experience, such as hallucinations and delusions. Meanwhile, negative symptoms refer to the lessening of normal functions related to motivation and verbal sociability.
Although atypical antipsychotics are becoming more common, they do have some side effects. The difference is that they have a lower risk of neurological side effects, as most of the SEs are metabolic, such as weight gain and hyperglycemia.
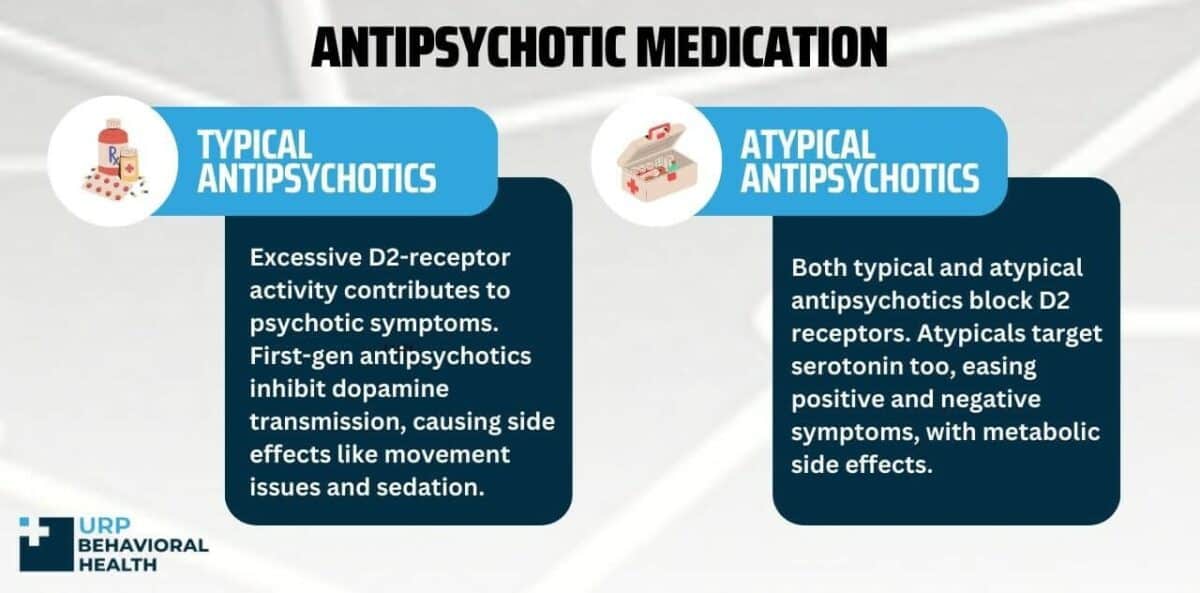
Antidepressants
This class of medications works by balancing the levels of neurotransmitters, which have an impact on mood and emotions. Early studies on these medications show that people who experienced improved moods faced changes in the levels of monoamines. Thus, healthcare professionals recommended the chemical imbalance theory, according to which insufficient monoamines cause depressive symptoms.
SSRIs
Antidepressants can address the issue by increasing the levels of monoamines in the brain. Selective serotonin reuptake inhibitors, commonly referred to as SSRIs, work by blocking the reabsorption of serotonin. This leaves more levels of the neurotransmitter in the synapses, alleviating symptoms of a major depressive episode. Other types include:
SSRIs
Serotonin and norepinephrine reuptake inhibitors can stabilize levels of serotonin and norepinephrine in the brain. Both these neurotransmitters have effects on memory, sleep-wake cycle, and, most importantly, mood. Hence, SNRIs work by inhibiting the presynaptic neuronal reuptake of norepinephrine and 5-HT once they’re released from the synaptic cleft. Thus, these monoamines remain in the central nervous system and alleviate symptoms.
TCAs
Tricyclic antidepressants are an older type of antidepressant, so they’re no longer used as commonly as other types, such as SSRIs. They function in a similar way to SSRIs; in that, they increase levels of serotonin in the synaptic cleft. But TCAs can be dangerous if taken in excess.
That’s because newer types are well-tolerated compared to TCAs, which can also lead to more unpleasant side effects. However, mental health practitioners may prescribe them if you don’t respond to other antidepressant medications.
MAOIs
Just like other types, monoamine oxidase inhibitors work by affecting the brain chemistry that’s associated with depressive symptoms. These drugs target monoamine oxidase, an enzyme that’s involved in reducing the levels of dopamine, serotonin, and norepinephrine in the brain. When MAOIs work, they prevent this from happening, which leaves higher levels of neurotransmitters available.
However, these can also lead to side effects, such as headaches, insomnia, dry mouth, and nausea. Moreover, taking these antidepressants will require you to make certain diet restrictions and avoid other medications that can potentially react with the MAOIs.
Mood Stabilizers
When you develop the bipolar subtype of schizoaffective disorder, you experience manic and depressive episodes in addition to psychotic symptoms. In this situation, providing antidepressants to counter depressive symptoms can be dangerous as higher concentrations of neurotransmitters can lead to a manic episode.
Medical researchers have found that bipolar mood fluctuations occur due to a neurochemical imbalance. This results in heightened brain activity and subsequent manic episodes. Therefore, mood stabilizers are prescribed as a way to restore that balance and prevent extreme highs and lows. The most commonly used mood stabilizers include carbamazepine, valproic acid, and lithium.
FAQs
Some commonly asked questions regarding schizophrenia include:
Mental health practitioners at URP Behavioral Health treat schizoaffective disorder using a combination of medication, evidence-based therapies (individual psychotherapy, family therapy, group therapy), and holistic therapies.
Mental health professionals diagnose schizoaffective disorder using the criteria provided in the APA’s DSM-5 and the WHO’s ICD-11. It lists specific symptoms that you have to show in order to receive a diagnosis.
Psychiatrists prescribe antipsychotic medication to manage symptoms such as hallucinations and delusions. They may also prescribe antidepressants if you have the depressive subtype of the disorder. And if you have the bipolar subtype of schizoaffective disorder, you’re prescribed mood stabilizers to prevent a manic episode.
References
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/antipsychotic-medications
- https://pubmed.ncbi.nlm.nih.gov/3059473/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC167197/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2838993/
- https://pubmed.ncbi.nlm.nih.gov/30642415/
- https://www.sciencedirect.com/science/article/abs/pii/S0378608022000332
- https://www.sciencedirect.com/topics/nursing-and-health-professions/typical-antipsychotic
- https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/typical-antipsychotic
- https://www.ncbi.nlm.nih.gov/books/NBK519503/
Let Us Guide You Towards Healing
We know that seeking treatment can be overwhelming, but our staff is here to make the process as smooth as possible. We’re available 24/7 to address any questions or concerns you may have.